That deep, throbbing ache at the back of your jaw is unmistakable. It can strike suddenly, turning the simple act of chewing or even smiling into a painful ordeal. Whether it’s the initial eruption in your teens or a sudden flare-up decades later, the discomfort demands one pressing question: how long must this last? The answer isn’t simple, as the duration hinges entirely on the root cause. Understanding the different timelines for various types of discomfort is crucial for managing your expectations and, more importantly, for recognizing when that nagging ache is a signal to seek immediate professional help. Navigating the complexities of wisdom tooth pain requires a clear map of its potential journey from a minor irritation to a major dental emergency.
Decoding the Discomfort: It’s Not Just One Type of Pain
Before we can talk about duration, we must first identify the source. Wisdom tooth pain isn’t a monolithic experience; it manifests in distinct ways, each with its own clock.
- The Pain of Eruption: This is the classic, dull, persistent ache that accompanies the tooth’s attempt to break through the gum tissue. It’s caused by the pressure of the tooth against your gums and jawbone and the subsequent inflammation as the gum tissue stretches and tears slightly. Think of it like teething, but for adults.
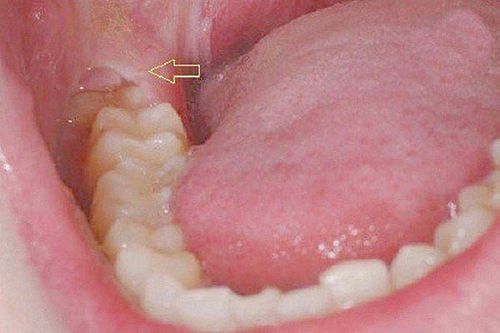
- The Pain of Impaction and Infection: This is a different beast altogether. It occurs when a tooth fails to erupt fully (becoming impacted), creating a flap of gum tissue that traps food debris and bacteria. This leads to a condition called pericoronitis—an infection characterized by sharp, severe pain, intense redness, swelling, and often a terrible taste in your mouth or even pus. This pain is acute, intense, and a clear sign of a problem that won’t resolve on its own.
The Timeline of Wisdom Tooth Pain: From Days to a Lifetime
So, how long does each type actually last? The spectrum is wide, ranging from a few days to a recurring nightmare.
Short-Term Pain: The Eruption Ache
For a lucky minority, the discomfort of a wisdom tooth cutting through the gums is a temporary nuisance. This type of pain typically comes in waves. You might experience a few days of noticeable aching and tenderness, followed by a period of respite as the tooth pauses its movement. This cycle can repeat over several weeks or even months until the tooth fully emerges—if it ever does. The acute phase of any single “eruption wave” usually subsides within three to seven days. During this time, the pain is manageable with over-the-counter pain relievers, saltwater rinses, and a soft diet. It’s unpleasant but often not sinister.
Long-Term and Recurrent Pain: The Pericoronitis Cycle
This is where the situation becomes chronic. An infection like pericoronitis might seem to get better with improved oral hygiene or a course of antibiotics, but this is often just a temporary ceasefire. Because the underlying anatomical issue—the partially erupted tooth and the gum flap—remains, the pocket where bacteria thrive is still there. This sets up a vicious cycle: the area becomes infected, causing pain and swelling; treatment calms it down; then, a tiny piece of food or a slight dip in your immune system triggers another infection. This cycle can repeat every few weeks or months for years, making the pain a permanent, looming presence in your life. It doesn’t “last” continuously, but it keeps coming back, which is arguably worse.
Pain After Extraction: The Healing Process
If you choose the route of removal, you’re trading one type of pain for another—a finite, healing pain for an indefinite, problematic one. Post-operative pain and swelling are normal and expected. The most intense discomfort usually occurs within the first 24 to 72 hours after the procedure. Significant improvement is typically seen within a week, and any lingering soreness or stiffness in the jaw usually resolves within ten to fourteen days. This timeline is a planned recovery, a direct investment in a future free from wisdom tooth problems.
When Should You Worry? The Red Flags That Demand Action
While some ache is expected, certain symptoms are major warning signs that indicate a complication requiring immediate dental attention. Do not dismiss these.
- Pain That Lasts Beyond the Normal Timeline: If post-extraction pain suddenly intensifies after the first three days instead of improving, it could be a sign of a dry socket (alveolar osteitis), where the blood clot dislodges, exposing bone and nerves.
- Signs of Spreading Infection: This is a serious medical concern. Symptoms include:
- Fever and chills.
- Difficulty swallowing or breathing.
- Swelling that continues to grow, especially if it spreads to your cheek, neck, or eye.
- Pus discharge from the socket or gums.
- Persistent Numbness: Lingering numbness (paresthesia) in your tongue, lip, or chin beyond the effect of the local anesthetic could indicate nerve involvement and needs immediate evaluation.
- Uncontrolled Bleeding: While some oozing is normal after an extraction, active bleeding that refuses to subside after applying firm pressure with gauze for 20-30 minutes is a problem.
- A Persistent Bad Taste or Smell: This is a classic sign of an infection or food trapped in a socket that isn’t healing properly.
If you experience any of these symptoms, contact your dentist or oral surgeon immediately. Do not wait for your scheduled follow-up appointment.
Managing the Pain and Protecting Your Health
For temporary eruption pain, management is key. Saltwater rinses (½ teaspoon salt in warm water) reduce inflammation and cleanse the area. Over-the-counter anti-inflammatories like ibuprofen can effectively tackle both pain and swelling. A soft diet avoids further irritating the tender gums.
However, for recurrent or severe pain indicative of impaction or infection, management is not a solution. Masking the pain with medication does nothing to address the root cause. The only way to break the cycle and achieve permanent relief is to remove the source of the problem. Consulting a dentist for a panoramic X-ray provides a definitive view of your wisdom teeth’s positioning, allowing for a clear diagnosis and a confident treatment plan.
Conclusion: Listening to Your Body’s Signals
Wisdom tooth pain is a messenger. Short, manageable bouts of ache might simply be announcing a tooth’s arrival. But persistent, severe, or recurring pain is an urgent distress signal, warning of infection, impaction, or damage to other teeth. Ignoring this signal can lead to cysts, gum disease, and the decay of adjacent healthy molars. Understanding the difference between normal discomfort and a serious complication empowers you to take the right action at the right time. Trusting professional expertise, such as that provided by clinics like Nuffield Dental, ensures that you receive an accurate diagnosis and a treatment plan tailored to your long-term health, finally putting a stop to the cycle of pain. Don’t just endure the ache—decode its message and take the steps toward a permanent solution.
Frequently Asked Questions (FAQs)
- Can wisdom tooth pain come and go?
Absolutely. This is the hallmark of pericoronitis. The pain flares up during an active infection, subsides with cleaning or antibiotics, and returns weeks or months later when bacteria become trapped again.
- Is it normal for wisdom tooth pain to cause headaches and earaches?
Yes, this is common. The pain from your jaw joint and molars can refer along nerve pathways to your head and ear, manifesting as a dull headache or an earache without an ear infection.
- How can I tell if my wisdom tooth is infected versus just erupting?
Eruption pain is typically a dull, pressure-like ache. An infection (pericoronitis) is usually sharp, severe, and accompanied by visible signs like bright red, swollen gums, a bad taste, pus, and swelling in the cheek or jaw.
- Can a wisdom tooth cause pain years after it came in?
Yes. A tooth that erupted straight might later become harder to clean as you age, leading to decay or gum disease. Alternatively, a slowly shifting tooth can start impacting the neighbor years later.
- What happens if I never get my painful wisdom teeth removed?
Chronic infection can lead to bone loss around the tooth, damage to the roots of the adjacent molar (often requiring a root canal or extraction on that tooth as well), and in rare cases, the formation of cysts that can destroy large portions of the jawbone.